Leeches and the Legitimizing of Folk-Medicine

“Men would rather pop Viagra forever than let a leech near their body,” Dr. Andrei Dokukin says with only a hint of hyperbole. From his Long Beach, California, clinic, Dokukin is one of the only medical doctors in America practicing leech therapy (also known as hirudotherapy) for internal medicine and non-surgical conditions. While his clients are treated for chronic pain, arthritis, and circulatory issues, rather than erectile dysfunction, Dokukin notes that ED could, in fact, be successfully remedied by using leeches to improve blood flow to such tissue. “If people were more accepting, I’d have a line around my office,” he speculates.
Dokukin, an alcoholic in recovery, received leech therapy himself to treat his liver cirrhosis. Before turning to hirudotherapy, he was offered few other choices. “We don’t have anything for liver diseases in this country besides liver transplant,” he says. “Or, basically, we can wait and see or die.” Underwhelmed by either option, Dokukin tried hirudotherapy at the behest of his mother back in Russia, where it remains common practice. Five years later, he claims that his liver has fully compensated and that his Western doctors are “astonished” by his recovery.
Dokukin’s experience illustrates westernized medicine’s hesitation to accept leeches as a legitimate therapeutic. When it comes to folk remedies, it can be challenging to extricate the science from pseudoscience. Leeches have been used across centuries and cultures to treat a litany of conditions, from hemorrhoids and fevers to psoriasis and tinnitus. The sheer range of purported applications, as well as a history steeped in spirituality and mysticism, makes it easy for skeptics to dismiss hirudotherapy as unscientific.
But while traditional notions of leeches restoring “bodily harmony” might strike the modern reader as hokum, they carry a shred of truth; leeches do indeed work for a wide range of conditions. Leeches not only draw contaminated blood from the body but also inject the surrounding tissue with various molecules that have been proven to decrease inflammation.

The problem, however, is that we don’t know just how well they work. Despite leeches’ having gained FDA approval as a medical instrument in 2004, a frustrating lack of clinical evidence persists. The most commonly cited review, for example, does not compare the use of leeches to non-leeches in surgical reconstruction, itself noting an “absence of robust randomized controlled trials on which the evidence may be based.”
Still, it would be a mistake to write off leech therapy as an ancient tradition of little worth. Many highly beneficial modern treatments, from bacteriophage therapy to cancer drugs, began their journey as “folk remedies.” These, too, battled both the Western standard of evidence and its biases. Yet as we have learned more about the molecules and mechanisms responsible for their efficacy, we have come to recognize their brilliance.
It's time we do the same for leeches.
{{signup}}
The Biology of the Leech
The medicinal leech, Hirudo medicinalis, is a remarkable creature. A hermaphroditic segmented worm belonging to the phylum Annelida and cousin to the more familiar earthworm, these animals have a sleek, sucker-tipped body resembling a cross between a trilobite and a slug. Leeches spend their days in freshwater ponds, marshes, and slow-moving streams across every continent except Antarctica, gliding along submerged vegetation, clinging to passing hosts, and feeding on the blood of fish, amphibians, and sometimes mammals.

A closer look at Hirudo medicinalis reveals what is essentially a highly optimized tube. This tube is replete with two sets of specialized suckers at each end of the leech’s body. The posterior sucker — the larger and more muscular of the two — aids in movement, vaulting the animal forward by gripping the terrain ahead. The anterior sucker, surrounding the mouth, contains the feeding apparatus. This anterior region also houses five pairs of eyes that allow the leech to detect light, movement, and potential hosts. The leech’s mouth contains three saw-like jaws arranged in a Y-shape, each bearing approximately 100 sharp teeth. These jaws create a characteristic bite — an inverted Y inside a circle — that is a telltale sign of leech feeding.
Only 15 species of leech, out of about 600 known species, are used in medicine.1 Their saliva contains over 20 bioactive compounds, including hirudin, a powerful anticoagulant. Leech saliva also contains anti-inflammatories, vasodilators, antibiotics, and hyaluronic acid, which helps break down tissue barriers, thus allowing other molecules to spread more effectively through the body.
The Ancient Origins of Hirudotherapy
While it would take until the late 19th century to begin to clarify the mechanisms behind their biology, leech therapy stretches back to the cradle of civilization. The earliest documented evidence of leech therapy appears in ancient Eastern medical traditions, where theories of bodily balance emerged independently across multiple civilizations.
In ancient China, leech therapy is mentioned in the Shennong Bencaojing, a 3rd-century CE book of traditional Chinese medicine, where medicinal leeches (Shuizhi) were recognized for their anti-coagulatory and anti-inflammatory effects. Chinese medicine developed around the concept of qi, the vital energy that flows through the body, and the balance between yin and yang forces. Disease was understood as a disruption of this harmony, and leeches were employed to address stagnant blood and restore energy flow. Unlike the medical traditions that would follow, however, this was not done through drainage with live leeches but through dried leech preparations that were either decocted and consumed like a tea or used as a topical ointment.
In India, leech therapy, or Jalaukavacharana, has been a cornerstone of Ayurvedic medicine for millennia. According to historical records, the practice dates back approximately 3,500 years, with the god of Ayurveda, Dhanvantari, often depicted holding a leech. Detailed protocols are preserved in ancient texts, such as the Sushruta Samhita (100-600 BCE). In Ayurveda, leech therapy focuses on treating "Pitta disorders," conditions involving blood or heat imbalances of "vata, pitta, and kapha” (air, fire, and earth).
Eastern observations that bodily functions followed discoverable laws and that targeted interventions could restore health traveled westward, profoundly influencing Greek medicine. Hippocrates (460-370 BCE) adapted these ideas into what became Western humoural theory, proposing that health depended on balancing four humours.
“Disease was understood as a state of imbalance or dyskrasia between the humours that made up the body’s krasis, its general constitution or complexion. Curing a disease meant rectifying the imbalance within the organism by returning the humours to their proper mixing, or eukrasis,” writes historian Noga Arikha in her book Passions and Tempers: A History of the Humours. These four humours were blood, phlegm, black bile, and yellow bile. Leeches were employed to restore balance by removing “bad” or excess blood, which dominated these other fluids.
The ancient surgeon Galen (130-201 CE) formalized these concepts into a system that would shape Western medicine for nearly two millennia. He developed intricate protocols for determining exactly how much blood should be removed, from which body parts, based on the patient's age, constitution, the time of year, and even the weather. Leeches were preferred over surgical bloodletting because they removed more controlled amounts of blood.
Centuries later, in his 1870 medical encyclopedia, American Dispensary, American physician John King remarked that leeches were better suited for “children and delicate adults” not to mention delicate tissues “… when it is required to abstract blood from some part whose locality or sensitiveness contra-indicates the lancet or cupping … [such as] … hemorrhoidal tumors, prolapsed rectum, inflamed vulva … watching that they do not creep out of reach within any of the internal cavities of the body."
Indeed, Napoleon Bonaparte would employ leeches to treat his hemorrhoids during military campaigns. This practice was encouraged by Napoleon's physician, François Joseph Victor Broussais (1772-1838), who became such an ardent supporter of leeching that he earned the nickname the "vampire of medicine." It was said that Broussais prescribed an application of 30 leeches to each new patient regardless of their diagnosis.
“Such was the zeal for leeching,” write historians of science Kirk, Pemberton, and Serviant-Fine, “that nineteenth-century Parisian hospitals maintained large quantities of leeches in purpose-built pools.” In a span of only a few decades, demand from the city began to eradicate leeches from the rural marshlands of France, and by 1827, France was importing 33 million leeches per year with an estimated value of Fr. 1,009,000 francs.
Supplies became so limited worldwide that, in the U.S. in 1835, a $500 reward was offered to anyone who could successfully breed European leeches.2
Yet by the turn of the century, leech mania had waned. With prominent scientists such as Louis Pasteur decrying bloodletting, and the rise of germ theory and treatments based on microbiology, leeches were losing their place as the pharmacopeia modernized. Only a few true believers lamented the loss of the leech and the bloodletters who utilized them. The British clinician Charles Hare wrote in his book, appropriately titled Good Remedies, Out of Fashion, that bloodletters are "no more found in the Post Office Directory, than …the Dodo or the Ichthyosaurus." Indeed, by the 20th century, the leech had gone from inspiring patterns on textiles and poetry to a largely obscure medical relic.
Why the Leech Works
Although widespread use of the annelid itself had fallen out of fashion, scientists continued to seek out the molecule or substance responsible for the leeches’ seeming efficacy.
The search began when British physician John Berry Haycraft first observed the antithrombotic quality of leech saliva. In a paper presented to the Royal Society in 1884, Haycraft speculated that " … the leech secretes some … juice which antagonises the blood ferment, preventing coagulation within its body."
Further investigating the action of this substance in the blood, Haycraft conducted a series of experiments in which he soaked leech pharynxes in alcohol for three days, then used water to extract a clear, alkaline fluid almost free of all other proteins and compounds. Adding this fluid to the blood of cattle, he confirmed that even small amounts of leech extract could prevent coagulation for hours.
While Haycraft was the first to explore this “leech extract” systematically, he had not yet narrowed in on the molecule responsible. This honor belongs to the German pharmacologist Carl Jacoby. In 1905, Jacoby was also experimenting with ways to isolate the anti-coagulant from the leeches’ salivary glands. His process involved grinding up the leech, which was then diluted in a saline solution. This mixture was filtered before being briefly heated, chilled, and centrifuged to precipitate any proteins. The resulting material was decolorized (which removes unwanted chemicals) by a talc filtration before being dialyzed to remove salts.3 Jacoby called the final product “hirudin.”
Even with hirudin identified, researchers still needed to characterize how the molecule worked and, if they ever hoped to synthesize it, how it was structured. The first step came in 1957, when the German pharmacologist Fritz Markwardt reported that he had finally succeeded in isolating hirudin in pure crystalline form.4 However, the complete amino acid sequence wasn’t determined until 1984 by Johannes Dodt and his team at the University of Munich. Their research revealed hirudin as a compact molecule — a small protein made of just 65 amino acids.
With its structure determined, researchers could finally decipher hirudin's mechanism of action. This, it turned out, was highly related to its structure and works by blocking an enzyme in the blood that facilitates blood clotting, called thrombin. One end of hirudin locks directly into thrombin's catalytic site (the part that normally cuts blood proteins), while the other binds onto the enzyme's surface and prevents the activation of other clotting factors. What's more, this binding is so tight that it seldom lets go under normal, bodily conditions.
The next breakthrough in understanding the pharmacological activity behind leech therapy came with the ability to synthesize hirudin. By 1988, scientists were able to produce recombinant hirudin in sufficient quantities for clinical use, bypassing the need to extract it from thousands of leeches. This leap enabled the development and marketing of several hirudin-based anticoagulant drugs, such as lepirudin (Refludan), desirudin (Revasc/LPriVask), and bivalirudin, each with slight modifications for improved safety or efficacy.
While pharmaceutical companies focused on hirudin synthesis, surgeons and engineers recognized that understanding the leech's mechanical function offered potential for more site-specific therapeutics. While broad-acting anticoagulants help prevent systemic blood clotting, there are many occasions that call for targeting localized areas, such as in reconstructive surgery involving the breast, nose, or digits. Dr. Jayant Agarwal, head of the Division of Plastic Surgery at the University of Utah School of Medicine, uses leeches to address venous congestion — a dangerous condition where excess blood pools in the tissue and can lead to necrosis if not addressed promptly. "If there's a pooling of blood, or the venous system is not functioning properly, the tissue can't get new, fresh oxygen or nutrients, and it has a harder time healing and surviving,” Agarwal says.
When tissue is reattached or transplanted, arteries tend to reconnect more readily than veins, often leading to venous congestion. Medicinal leeches provide a simple yet effective solution. When attached to such tissue, leeches suck out surplus venous blood, enabling freshly oxygenated blood to enter and nourish the area until it heals on its own.
The clinical results that do exist seem promising: in a 2012 study that reviewed 277 reported clinical cases of hirudotherapy in plastic and reconstructive surgery, researchers demonstrated a total tissue salvage rate of 78 percent. The case reports found leeches especially useful in aiding the salvage of replanted extremities and free tissue transfer — the transfer of tissue surgically detached from its original blood supply and transplanted to a new location, where it is reconnected to new blood vessels. While a later study from 2017 placed the overall success rate lower (61 percent) due to differing success criteria,5 leeches proved especially effective for indications like those involving “free flaps,” where their success rate was 70 percent.
Validating these results would take more systematic studies with robust controls. Even so, there are reasons to trust such findings, given what we know about hirudin and its effect on blood flow. The cause for skepticism, then, would pertain to potential downsides.
Infection remains the most serious of these, as the leech's digestive tract contains several bacterial species that contribute to the digestion of ingested blood. A 2024 study on infection after microsurgical breast reconstruction reported that, out of 34 adverse reactions, six patients presenting with infections produced cultures specific to leech pathogens, confirming hirudotherapy as the cause (17.6 percent). While this is a small sample size, it is consistent with longitudinal studies on hirudotherapy-driven infection in venous flap reconstruction, which show infection rates of 2.4 percent to 20 percent.
Beyond the risk of infection, there are handling and maintenance challenges that complicate working with leeches. It takes around two years for leeches to mature to the point of medical use. In this period, they are fed on sheep's blood up until about six to nine months before application, at which point they are starved to ensure their guts are empty. While their storage needs are fairly simple — buckets of desalinated water changed daily — they are still live animals with specific requirements. Accustomed to silty riverbeds, for example, leeches prefer cool temperatures out of direct sunlight. And while they are comfortable sharing space, no more than 50 leeches should occupy a 2.5-liter container.
Wanting to capitalize on the leech’s sucking mechanism while avoiding the drawbacks of live leeches, scientists began to prototype artificial suction devices as early as the nineteenth century. Jean-Baptiste Sarlandière invented a mechanical blood pump in 1817, intended to allow a precise suctioning of blood from the human body. In an 1819 pamphlet, he outlined specific drawbacks he hoped his bdellomètre would address, among them, how: “after the application of a certain number of leeches it was never possible to determine exactly how much blood had been evacuated … [nor] … the rate of the flow of blood.” In 1840, a French surgeon, Baron Charles Louis Heurteloup, developed a spring-loaded version, especially designed for veins around the eyes.
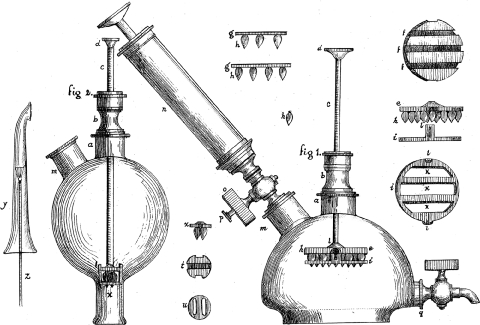
Despite never achieving widespread adoption, mechanical mimics persisted. Compared to their heavier predecessors, with their metal discs and pistons, 21st-century versions resemble small plastic combs with fine needles for delivering anticoagulants. In 2001, researchers published the results that a mechanical prototype had achieved a 60 percent tissue survival rate compared to just 34.6 percent with biological leeches.6
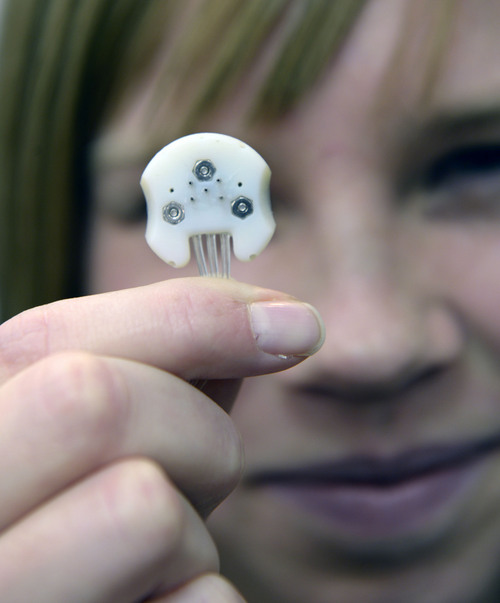
Dr. Agarwal has been working on a mechanical leech system in collaboration with Dr. Bruce Gale, a Professor in Mechanical Engineering at the University of Utah, and a team of engineering students since 2013. The patented prototype simultaneously removes blood from congested tissue and delivers anticoagulants like heparin through multiple hollow needles that penetrate the skin. Its precision is a key advantage. "We can control the anticoagulant delivery and simultaneously control negative suction and blood removal,” says Agarwal.7
Despite the promise of such devices, these research groups continuously fail to secure funding for the wider testing, production, and deployment of such devices. "The use of leeches,” Argawal explains, “is very niche and not a huge market, so there are not a lot of agencies or investors interested in funding the development of a mechanical leech.”
Good Remedies, Back in Fashion
That the data supporting leech therapy remains so anemic is ironic given the legacy of widespread medicinal leech use and its continued use today.
In modern India, Ayurvedic leech therapy employs a precise three-step process that looks very similar to those administered centuries ago: leeches are first purified in turmeric water for approximately 45 minutes to activate them, then applied to cleaned skin, where they attach and feed for 30-50 minutes before detaching naturally. This is followed by post-treatment care, including turmeric application to stop bleeding. Dr. Suneera Banga at Maharishi Ayurveda Hospital in New Delhi has treated over 300 patients over seven years, with treatment courses of 5-7 sessions. "Leech therapy is very common for Indian people," she notes, even among highly educated demographics that could afford the comparable pharmaceuticals more common in the West.
Russia has likewise maintained this tradition. In 2009, Russia bred 10 times more leeches than the rest of the world combined, and by 2017, about 10 million leeches were prescribed to patients every year, often as low-cost substitutes for blood thinners.
A similar story plays out across the Caucasus in Georgia, where leech therapy is prescribed for everything from varicose veins to high blood pressure. In Tbilisi, leech therapists operate out of day spas and medical clinics, sourcing their leeches from regional bio-farms and blending modern pharmacology and traditional techniques. Some practitioners even claim that leeches can “diagnose” blood problems and adjust their saliva accordingly, a belief that echoes folk wisdom found across Eurasia.
In the UK, Bridget Croft, a general and obstetric nurse, now runs a leech clinic in the Midlands after training in Germany at an institute dedicated to certifying hirudotherapists. On her website, she notes that while less popular in England, “Leech therapy has never gone out of use to treat a myriad of disorders and enhance wellbeing in the Middle East and in Eastern Europe.” And to challenge the ick-factor, Croft presents videos showing relaxed patients hosting multiple leeches in a clinic that looks as “modern” as any other, with computers, beakers, and surgical paraphernalia. Patients, from pensioners to musicians, offer testimonials to the treatment’s effectiveness for conditions ranging from whiplash to osteoarthritis.
One of the most striking things about live leech therapy, as it is practiced in these clinics, is its accessibility. While the patented molecules may be costly, hirudotherapy in its simpler form — live leeches applied directly to the skin in a small clinic — is not. Leech therapy in India costs as little as $1.50 - $11.5 per session, while in the UK, Croft charges £195 for an initial consultation and £175 for follow-up sessions. Even in the U.S, the therapy is relatively inexpensive; a treatment with Dr. Dokukin begins at $250 per session. “I don't practice it for profit,” he says.

Affordability, however, is not the only reason people seek out hirudotherapy over more conventional modern alternatives. Sometimes, they are driven to it because, as with Dr. Dokukin’s liver damage, limited treatment options exist for their condition.
The problem is that the efficacy of live leech treatment is still woefully under-researched, whether owing to lack of investment, research infrastructure, continued Western hesitancy, or some combination of these.
While proponents of hirudotherapy claim that “Medical leeches significantly improve the prognosis of liver disease,” there is a dearth of credible support. A study from 2020 concludes that while participants reported improvements in health immediately after therapy, leech-based “detoxification therapy did not have a significant effect on the regulation of established levels of blood components …” The authors did, however, mention that they only conducted one cycle of treatment and that more research would be needed.
Findings for other conditions are more promising, though these claims, too, are underresearched. Arthritis and osteoarthritis are of particular interest as inflammatory conditions that relate to blood flow. Not only that, but current methods of treatment mostly focus on managing symptoms. “In the Western medical world,” Dokukin notes, “we inject our knees with steroids. We destroy the joints further. We use things like hyaluronic acid, which doesn't really work, or we replace the knees, which is an expensive operation.”
Auspiciously, in a 2018 meta-analysis of randomized controlled trials involving leech therapy, pain relief, and functional recovery in patients with symptomatic knee osteoarthritis, the authors concluded that the therapy “was associated with significantly improved outcomes.” However, they also advise that, due to a lack of evidence, this “conclusion should be interpreted cautiously.”
We need high evidentiary standards for medicine. However, it is worth considering the high cost of meeting them. A recent report from RAND estimated that the median cost of bringing a drug to market is $708 million. While this may be worth it for some hirudin-based drugs, live leech treatments are incredibly low-margin. Clinical studies on their efficacy are almost certainly a money-losing proposition. Interestingly, this same difficulty has accompanied other traditional treatments such as phage therapy.
Phages, like leeches, are a “natural biological substance,” which cannot be patented without evidence of “a new and inventive transformation.” Those who hope to make money on the therapy have thus turned to synthetic phages or bespoke phage products based on automated analysis of patients’ bacterial samples. These “are likely to work out in the region of $20,000 per treatment,” reports the writer Tom Ireland, and could very reasonably help pharmaceutical companies justify the high cost of clinical trials. The same cannot be said of Agarwal’s mechanical leeches, and certainly not the worm itself. And while hirudotherapy could draw inspiration from phages, bioengineering leeches to make them patentable and attractive for clinical trials would be likely to reduce the allure of their financial accessibility.
It may be some time before we can come up with robust evidence for the efficacy and safety of leech therapy. But that is not the crux of this story. People all over the world continue to use this treatment even in the absence of clinical evidence. It is mostly patients in the West who lose out. The story, then, is not only about evidence, but how we approach what we view as folk remedies. While not all treatments are equally effective, effective treatments can come from anywhere. We have seen this play out often enough that the very least we can do is show greater curiosity about the potential of leechcraft.
{{divider}}
Khushi Mittal is the founder and CEO of Observv Aviation, an India-based aviation company focused on manufacturing autonomous, amphibious airplanes in the 5-10 tonne capacity. She writes occasionally to find answers to three questions: Where are we right now? How did we get here? And how to get back to the future? You can follow her @khushhhi.
Xander Balwit is editor-in-chief of Asimov Press and a huge admirer of maligned creatures.
Cite: Mittal, K. & Balwit, X. “Leeches and the Legitimizing of Folk-Medicine.” Asimov Press (2025). https://doi.org/10.62211/94et-23dd
Acknowledgements: Thanks to Dr. Andrei Dokukin for his candor and for spending hours talking about leeches. Thank you also to Dr. Agarwal for the interview, as well as to Devon Balwit for additional historical research and Dr. Ella Watkins-Dulaney for helpful feedback and for making the lead image of this article.
{{divider}}
Footnotes
- A leech ready for medicinal use resembles “a rat’s tail with a thin and small head, red abdomen, and green back.”
- While the U.S. had indigenous leeches, they were smaller and supplied less blood.
- Like other early biochemical techniques, such as the extraction of insulin, these derivation processes were woefully inefficient and expensive. In the case of hirudin, some 50,000 ground leech heads per year were required to produce enough extract for research.
- If this were not achievement enough, he also characterized its binding to thrombin, noting that: “The effectiveness of hirudin can then be expressed in antithrombin units.” This allowed for the precise measurement of hirudin’s potency and the establishment of standardized dosing protocols, easing the way for reproducible clinical research.
- In Whittacker et al.’s study from 2012, “success” was defined as survival of the tissue/flap (even if a small amount of the flap needed debridement) whereas Cornejo et al. deemed something a successful therapy “only when no flap was lost or when the original reconstructive goal was achieved in spite of the amount of tissue lost.”
- A follow-up study in 2002 demonstrated that four different mechanical prototypes removed between 609 percent to 853 percent more blood than biological leeches, with the most advanced versions sustaining high blood removal rates for up to 4 hours through subcutaneous anticoagulation.
- More recently, in 2016, a group of bioengineering students at Texas A&M received a Surgery Medical Device Innovation Grant to investigate their own prototype, made with a 3-D printed polylactic acid (PLA) and silicon tubing, in vitro.
Always free. No ads. Richly storied.
Always free. No ads. Richly storied.
Always free. No ads. Richly storied.